The body mass index (BMI) is a standard health assessment tool in most healthcare facilities.
Although BMI has been used for decades as the gold standard for your health, it has been widely criticized for oversimplifying what it means to be healthy.
Many claims that BMI is outdated, inaccurate, and should not be used in medical and fitness settings.
This article tells you everything you need to know about BMI, its history, whether it is an accurate predictor of health, and its downsides.
What is the BMI?
BMI stands for Body Mass Index. It was developed in 1832 by a Belgian mathematician named Lambert Adolphe Jacques Quetelet. He created the BMI scale to quickly estimate the degree of overweight and obesity in a given population to help governments decide where to allocate health and financial resources.
Interestingly, Quetelet claimed that BMI was not useful for study at the individual level but rather to give a snapshot of the overall health. However, today, the body mass index is widely used to measure an individual’s health.
The BMI scale is based on a mathematical formula that determines whether a person is a “healthy” weight by dividing their weight in kilograms by their height in meters squared:
BMI = weight (kg) / height (m2)
Once the BMI is calculated, it is compared to the BMI scale to determine if it is within the “normal” weight range:
- Less than 18.5 low weight high
- 18.5-24.9 Normal weight Low
- 25.0–29.9 Overweight Low to moderate
- 30.0–34.9 Obesity class I (moderate obesity) High
- 35.0–39.9 Obesity class II (severe obesity) Very high
- Over 40 Obesity class III (extreme obesity) Extremely high
Based on this estimate, a healthcare provider may suggest health and lifestyle changes if you are not in the “normal” weight category. Although this can give the healthcare provider a snapshot of a person’s health based on their weight, it does not consider other factors such as age, gender, race, genetics, fat mass, muscle mass, and bone density.
More information on this source text For more information on the translation, the
Is the body mass index a good predictor of health?
Despite concerns that BMI does not accurately identify whether a person is healthy, most studies show that a person’s risk of chronic disease and premature death increases with a very low BMI – less than 18.5 (“Underweight”) or very high – greater than 30.0 (“obesity”).
For example, a 2017 retrospective study of 103,218 deaths found that those who had a BMI of 30.0 or more (“obese”) had a 1.5 to 2.7-fold increased risk of death after a 30-year follow-up (1).
Another study showed that those in the “obese” BMI category had a 20% higher risk of death from all causes and heart disease than those in the “normal” BMI category.
The researchers also found that those who were in the “underweight” or “severely obese” and “extremely obese” categories died an average of 6.7 years and 3.7 years earlier, respectively, compared to those in the “normal” BMI category. ”.
Other studies have shown that a BMI greater than 30.0 significantly increases your risk for chronic health problems, such as type 2 diabetes, heart disease, breathing difficulties, kidney disease, non-alcoholic fatty liver disease, and mobility problems.
Because most research shows an increased risk of chronic disease among people with obesity, many health professionals can use BMI as a general snapshot of a person’s risk. Still, it shouldn’t be the only diagnostic tool used.
Disadvantages of BMI
Even though research associates a low BMI (below 18.5) and high (30 or more) with more significant health risks, its use has numerous failures.
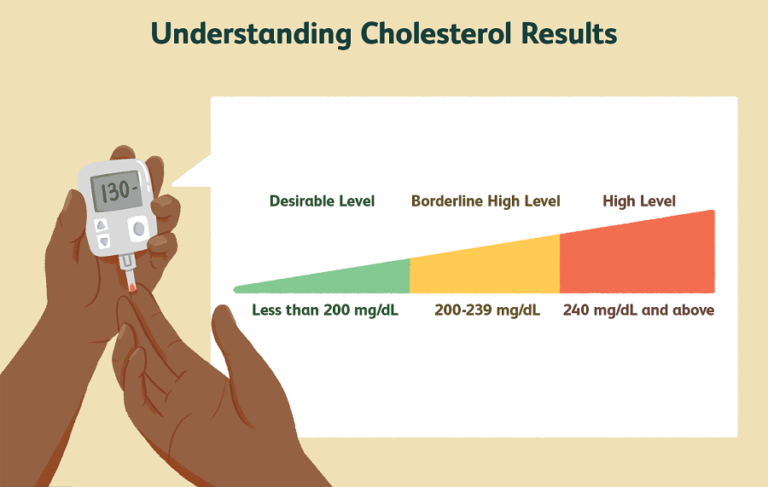
Relying solely on BMI can miss other necessary health measures, such as cholesterol, blood sugar, heart rate, blood pressure, and inflammation levels, and overestimate or underestimate a person’s proper health.
BMI also tells us nothing about where body fat is distributed. Body fat stored around the abdomen poses a greater health risk than body fat stored around the hips. This “apple” shape is associated with a higher chance of developing metabolic syndrome. This is a combination of related conditions, such as high blood pressure, high blood glucose, and high cholesterol levels, which increase the risk of heart disease, stroke, and type 2 diabetes.
Even though men and women vary in body composition, and men have more muscle mass and less fat mass than women, BMI uses the same calculation for both groups. Measuring waist circumference and body fat percentage may be more helpful in such cases.
Many people may have a “normal” BMI but are at increased risk for heart disease and type 2 diabetes based on blood pressure or body fat distribution.
Finally, simply by using BMI to determine a person’s health, other aspects of health are ignored, such as mental well-being and complicated sociological factors, such as income, access to affordable and nutritious food, dietary skills, and knowledge. And the living environment.
ABSTRACT
BMI is easy to measure and provides a rough estimate of disease risk. But while it’s a good starting point, BMI should be used in conjunction with other measures to get a complete picture of a person’s health risk. Lifestyle factors (such as smoking, physical activity, diet, and stress levels) and blood pressure, blood sugar, and blood cholesterol levels should be considered with BMI to establish health risks.
Additionally, using other body assessment tools in place of BMI, such as waist circumference and body fat percentage, can also help guide decisions about the best health interventions for a specific person. However, each has its own set of advantages and disadvantages.